Manage Parkinson s Diseases Without Medications: Leading Neurologist Shares Exclusive Tips
Can you manage Parkinson's disease without medication? Scroll down to see what a leading neurologist has to say.
 As we age, we are more prone to illness. While some of them can be tackled effectively others just make it challenging to cope with their consequences with every passing day. One such debilitating and devastating condition is called Parkinson’s disease - a degenerative disorder that affects the brain and the central nervous system. Often this condition affects the elderly population but at times can also catch up with the younger lot.
As we age, we are more prone to illness. While some of them can be tackled effectively others just make it challenging to cope with their consequences with every passing day. One such debilitating and devastating condition is called Parkinson’s disease - a degenerative disorder that affects the brain and the central nervous system. Often this condition affects the elderly population but at times can also catch up with the younger lot.
Parkinson’s disease is a neurodegenerative disorder and affects nerve cells which are responsible for motor functions of the body. Parkinson’s patients have difficulty in carrying out movements at a normal speed. Hence, they take longer to perform even normal day-to-day activities. Parkinson’s disease is found mainly in people over the age of 50 years and prevails in both the sexes. But if you consider the Indian statistics, it is more common in females than in males.
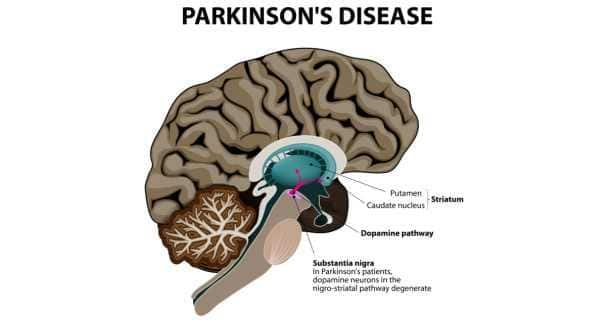
People with Parkinson’s disease suffer loss of nerve cells in the brain that are responsible for releasing a brain chemical or neurotransmitter called dopamine. Dopamine is a signalling chemical required for coordination and control of body movements.
Once the neurons start dying, the production of dopamine is reduced causing loss of movement control and coordination in people suffering from the condition. But what exactly triggers death of those neurons is still a mystery. Scientists have found out several genes that were responsible for causing the disease in some cases.
Large population studies have indicated that people who have a family member or a relative suffering from the disease have a higher chance of developing the condition themselves. However, this is just an observation and further research on the inheritance aspect of Parkinson’s disease is underway.
In Parkinson’s disease the basic characteristic symptoms are those of tremors (trembling or shaking), stiffness, and slowness of movement, these are called motor symptoms.
The non-motor symptoms might include difficulties in maintaining posture and balance, soft speech, problems with urinating, slow bowel movements and sleep disturbances. A characteristic of Parkinson’s is that the symptoms can change from day to day and sometimes even from hour to hour.
The motor symptoms in Parkinson’s are as follows:
Tremors: This happens usually in the limbs affecting the hands and feet but might sometimes also affects the lips, tongue, jaw, abdomen and chest. The tremors occur in the affected area when it is at rest and disappear during a movement. These tremors are often referred as resting tremors.
Rigidity: Rigidity of the muscle of the affected area is responsible for the aches and pains in the body. Such rigidity is called plastic or passive rigidity.
Bradykinesia: Slowness of bodily movements is termed as bradykinesia. This involves slowness in carrying out a movement, also hesitancy in initiating a new movement and fatiguing easily. There also appears to be a decrease in the performance of automatic movements like; eye blinking, swing of the arms while walking, hand gestures while talking, expressive facial movements etc.
Bradykinesia can also cause:
Although there are several tests like non-invasive diagnostic imaging tests that a neurologist uses to rule out the presence of other neurological conditions, there is no specific test that can confirm Parkinson’s disease. It is only based on individual description of symptoms and evaluation by a neurologist, a person is diagnosed of Parkinson’s. This the main reason why most cases of Parkinson’s go unnoticed.
Though Parkinson’s is not a life threatening condition it is definitely a life-altering condition. With the help of appropriate care and therapy, patients can lead a fulfilling life.
The most devastating part about Parkinson’s disease is that one has to live with this condition lifelong as it has no cure. But that shouldn’t refrain patients from seeking treatment. ‘A person with Parkinson’s requires various modalities of treatment along with medications,’ says Dr Maria Barrerto, CEO, Parkinson’s Disease and Movement Disorder Society.
Following are the ways in which Parkinson’s can be treated and controlled.
USING ORAL MEDICATIONS
Oral medications to a certain extent can help manage Parkinson’s symptoms. But remember as one ages and the disease advances, medication alone won’t be of help to control the symptoms. The effects of oral medications wane out with the progression of the disease but they are the first line of treatment in managing Parkinson’s disease. Some of the medications that might be prescribed to a Parkinson’s patients are as follows:
Levodopa: This medication is the most effective and primary medication prescribed to alleviate the Parkinson’s symptoms. Levodopa is a natural chemical that passes into the brain and is converted into dopamine, which then replenishes the deficiency of dopamine in the brain. By restoring dopamine it helps to regain motor functions, mobility and improves participation in the everyday activities. Side effects of Levodopa may include nausea and lightheadedness. Sometimes it can also give rise to involuntary movements if taken in higher doses. It is advisable to talk to the doctor immediately once such side effects are noticed.
Dopamine agonists: Unlike Levodopa, dopamine agonist doesn’t convert into dopamine but just mimics their effects and help in restoring brain functions. Dopamine agonist is used in conjunction to levodopa. Some of the side effects of dopamine agonists are similar to the side effects of levodopa, but it also includes hallucinations, swelling, sleepiness and compulsive behaviors such as hyper sexuality, gambling and over-eating. It is important for the caregiver to watch out if there is any out of character behaviour by the patient. Seek the doctor’s help to check on the doses.
Mono Amine Oxidase Type (MAO-B) Inhibitors: These medications help prevent breakdown of dopamine by inhibiting the enzyme monoamine oxidase which metabolizes dopamine. Side effects of this drug might include nausea or headaches. If used along with levodopa, these medications increase the risk of hallucinations too. These medications are not often used in combination with most antidepressants or certain narcotics due to potentially serious but rare reactions.
COMT Inhibitors: This medication mildly prolongs the effect of levodopa therapy by blocking an enzyme that breaks down dopamine. Side effects include an increased risk of involuntary movements leading to a condition called dyskinesias. This is basically a result of an enhanced levodopa effect. Other side effects include diarrhea or other levodopa side effects like nausea or headaches.
Anticholinergics: These medications were used for many years to help control the tremors associated with Parkinson’s disease. However, their modest benefits are often offset by side effects such as impaired memory, confusion, hallucinations, constipation, dry mouth and impaired urination.
Amantadine: This medication is prescribed to provide short-term relief of symptoms of mild, early-stage Parkinson’s disease. It may also be given with levodopa therapy during the later stages of Parkinson’s disease to control involuntary movements due to levodopa. Side effects may include a purple mottling of the skin, ankle swelling or hallucinations.
SURGICAL INTERVENTIONS
A surgical treatment is offered to patients who have reached the advanced stage of the disease and medication ceases to provide any relief to their symptoms. The surgical options those are available for Parkinson’s patients are:
Deep Brain Stimulation or DBS
In deep brain stimulation two surgically implanted medical devices called neurostimulators, similar to cardiac pacemakers are planted in the chest near the collarbone. These devices deliver electrical stimulation to precisely targeted areas on each side of the brain. Stimulation of these areas appears to block the signals that cause the disabling motor symptoms of Parkinson’s disease. As a result, many patients achieve greater control over their body movements.
A DBS system includes the following three components, which are implanted completely inside the body.
Neuro-stimulator: A pacemaker-like device is the power source for the system. It contains a small battery and a computer chip programmed to send electrical pulses to control Parkinson’s disease symptoms.
Lead: An insulated wire with four electrodes is implanted in the brain, with its tip positioned within the targeted brain area.
Extension: An insulated wire placed under the scalp that connects to the lead and runs behind the ear, down the neck, and into the chest below the collar-bone where it connects to the neurostimulator.
Once the system is in place, electrical impulses are sent from the neurostimulator up along the extension wire to the lead and into the targeted brain area. These impulses interfere with and block the electrical signals that cause Parkinson’s symptoms.
With the DBS one of two areas may be stimulated either the subthalamic nucleus (STN) or the internal globus pallidus (GPi). These structures are deep within the brain and involved in motor control. These structures control movement and muscle function. A neurosurgeon would determine which structure would be stimulated for the concerned patient.
While DBS can relieve some of the patient’s symptoms considerably it should be noted that it can target only some specific symptoms. It does not eliminate the use of drugs and medication nor does it result in the reversal of the PD symptoms.
Lesioning
This involves destroying or eliminating the specific part of the brain that is causing Parkinson’s diseases symptoms. However this surgery is rarely performed these days.
ADJUNCT THERAPIES
Apart from medications and surgery one might also be recommended certain lifestyle changes, especially to take aerobic exercises or other movement therapies. In some cases, physical therapy that focuses on balance and stretching also is important. ‘Parkinson’s treatment often needs a multidisciplinary approach, that includes therapies such as physiotherapy, speech therapy, occupational therapy, diet and nutrition, counseling, cognitive rehabilitation and creative therapies,’ says Dr Maria. The other additional therapies that might give respite to a Parkinson’s patient are:
Physiotherapy: This can help one manage mobility problem including gait, posture, balance dexterity etc. Physiotherapy would include exercises to improve mobility, help overcome side effects of medication and improve movement strategies.
Occupational Therapy: Occupational therapy promotes good health and well being by helping patients regain their independence and adapt to disability. It also uses practical aids to help one with various activities and ways to adapt to daily routine and surroundings. This therapy has to be designed differently for each Parkinson’s patient depending on their needs and severity of the condition.
Speech and Language Therapy or SLT: Speech and language therapy help patients communicate to the best of their ability by treating speech, language and communication problems. SLT also helps people in eating, swallowing and drooling problems too.
What do they do in speech and language therapy?
Can you manage Parkinson's disease without medication? Scroll down to see what a leading neurologist has to say.
A new research pointed out that practising the Chinese martial art could help curb and slow down the symptoms of Parkinson's disease.
Apomorphine has been found to be more effective in managing motor symptoms associated Parkinson's disease than other available medications.
Dispelling the myths and misconceptions about Parkinson's disease is important as these can prevent patients from receiving effective treatment and caring for themselves.
A Guide To Finding Quality Providers And Developing Effective Care Plans.
Although Deep Brain Stimulation (DBS) does not cure Parkinson's disease, it can ease the symptoms, reduce medication and enhance the quality of life
Studies have also shown how dogs sniffed bladder cancer in urine and detected lung cancer in exhaled breath
Parkinson's disease is a movement disorder that can hamper your daily activities. Read on to know if the disease is curable or not.
Cases of Parkinson's disease have been increasing rapidly, and experts believe that the best way to manage its symptoms is through timely intervention. Here's everything you need to know about the treatment of Parkinson's.
World Parkinson's Day is observed every year on April 11 to raise awareness about the disease. Here's everything you need to know about the disease and how it can be treated.
Currently, there's no cure for Parkinson's disease. But early diagnosis and treatment can lessen symptoms, improve one's quality of life, and prolong survival.
Parkinson's disease is a progressive nervous system disorder that affects the movement of your body. Some of the warning symptoms of this disease start gradually numbness of body parts, not able to move properly, etc.
A new study has found that energy deficiency is one of the major causes of Parkinson's disease. Read on to know how it increases your chances of developing the disease.
The study showed that the drug reduces the loss of dopamine neurons in females, which indicates it as potential evidence for the use of the drug to treat Parkinson's disease.
Men taking terazosin were 12 per cent to 37 per cent less likely to develop Parkinson's disease during follow-up than men taking tamsulosin.
There is now a scalpel-free alternative to brain surgery that can benefit patients with asymmetrical Parkinson's disease symptoms.
As we get ready to observe World Brain Day, learn to recognize the symptoms that indicate the early onset of Parkinson's so that you can delay the progress of the disease.
About 10 million people worldwide are estimated to be affected by Parkinson's disease, with higher incidence reported from the industrialized countries. Read to know about the new treatment procedures.
Can you manage Parkinson's disease without medication? Scroll down to see what a leading neurologist has to say.
A new research pointed out that practising the Chinese martial art could help curb and slow down the symptoms of Parkinson's disease.
Apomorphine has been found to be more effective in managing motor symptoms associated Parkinson's disease than other available medications.
Dispelling the myths and misconceptions about Parkinson's disease is important as these can prevent patients from receiving effective treatment and caring for themselves.
A Guide To Finding Quality Providers And Developing Effective Care Plans.
Although Deep Brain Stimulation (DBS) does not cure Parkinson's disease, it can ease the symptoms, reduce medication and enhance the quality of life
Studies have also shown how dogs sniffed bladder cancer in urine and detected lung cancer in exhaled breath
Parkinson's disease is a movement disorder that can hamper your daily activities. Read on to know if the disease is curable or not.
Cases of Parkinson's disease have been increasing rapidly, and experts believe that the best way to manage its symptoms is through timely intervention. Here's everything you need to know about the treatment of Parkinson's.
World Parkinson's Day is observed every year on April 11 to raise awareness about the disease. Here's everything you need to know about the disease and how it can be treated.
Currently, there's no cure for Parkinson's disease. But early diagnosis and treatment can lessen symptoms, improve one's quality of life, and prolong survival.
Parkinson's disease is a progressive nervous system disorder that affects the movement of your body. Some of the warning symptoms of this disease start gradually numbness of body parts, not able to move properly, etc.
A new study has found that energy deficiency is one of the major causes of Parkinson's disease. Read on to know how it increases your chances of developing the disease.
The study showed that the drug reduces the loss of dopamine neurons in females, which indicates it as potential evidence for the use of the drug to treat Parkinson's disease.
Men taking terazosin were 12 per cent to 37 per cent less likely to develop Parkinson's disease during follow-up than men taking tamsulosin.
There is now a scalpel-free alternative to brain surgery that can benefit patients with asymmetrical Parkinson's disease symptoms.
As we get ready to observe World Brain Day, learn to recognize the symptoms that indicate the early onset of Parkinson's so that you can delay the progress of the disease.
About 10 million people worldwide are estimated to be affected by Parkinson's disease, with higher incidence reported from the industrialized countries. Read to know about the new treatment procedures.
Living with Parkinson's can be a nightmare if you are alone. But, with our tips, you can have a better quality of life.
World Parkinson’s Disease Day on 11th April: Food dos and don’ts for the condition
Here's why you should never ignore loss of smell!
You will be surprised to know how hiccups could be a symptom of brain tumours, Parkinson's disease, esophageal cancer and these seven other chronic conditions.
Excessive iron intake can cause heart disease, osteoporosis, cancer + 3 more health conditions.
Aerobics exercises can significantly improve your health, and not just because it helps in weight loss! Here are six ways it can help in improving your emotional and physical well-being.
8 things you didn't know your smartphone could do (Slide Show)
Did you know that cinnamon has a key role in the treatment of Parkinson's disease? Here's more you should know about!
7 tips to live well with Parkinson's disease
The boxer's wife Lonnie shares some tips for caregivers as well.
Watch how Parkinson's affects your brain and other body functions.
In this video, Karen Rose, diagnosed with Parkinson's at the age of 34, talks about the impact of the disease on her life.